A paradigm shift in lipid management – „the sooner, the lower, the better“
Authors:
Dr. rer. medic. Kapka Miteva, PhD1
Priv.-Doz. Dr. Konstantinos C. Koskinas2
Prof. Dr. med. François Mach3
1 Department of Cardiology, Foundation for Medical Research, Faculty of Medicine, University of Geneva
2 Department of Cardiology, Bern University Hospital - INSELSPITAL, University of Bern
3 Department of Cardiology, Geneva University Hospitals, Geneva
Corresponding author:
Prof. Dr. med. François Mach
E-Mail: francois.mach@hug.ch
Vielen Dank für Ihr Interesse!
Einige Inhalte sind aufgrund rechtlicher Bestimmungen nur für registrierte Nutzer bzw. medizinisches Fachpersonal zugänglich.
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
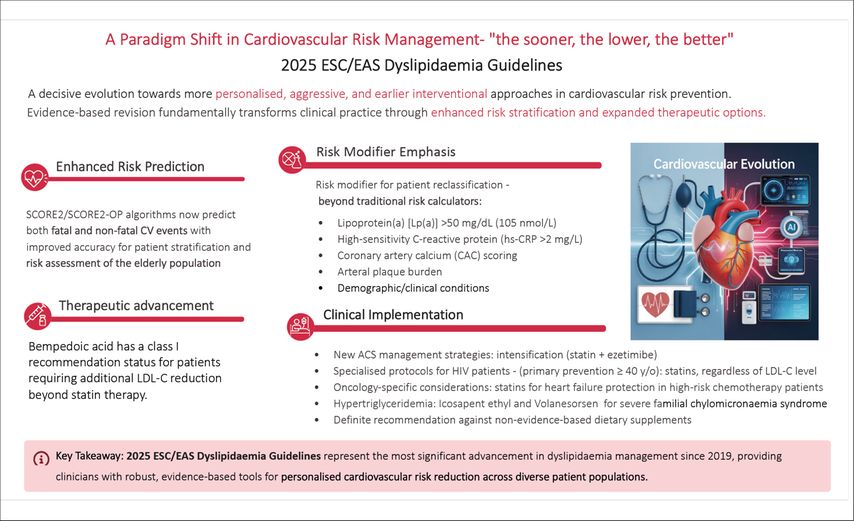
The 2025 Focused Update of the 2019 ESC/EAS Guidelines for the management of dyslipidaemias marks a significant evolution in cardiovascular (CV) risk prevention, and it delivers nothing short of a paradigm shift. Incorporating new evidence from major trials up to March 2025, this update moves decisively towards a more personalized, aggressive, and earlier interventional approach.
Key changes include the adoption of the SCORE2/SCORE2-OP algorithms for both fatal and non-fatal event prediction, a stronger emphasis on risk modifiers for patient reclassification, and a significant expansion of treatment options, including a Class I recommendation for bempedoic acid. This update provides clinicians with evidence-based strategies to achieve lower LDL-C targets sooner (Fig. 1). In particular, it provides the practicing clinician with new strategies for managing acute coronary syndromes, specific populations like people with HIV (PWH) and oncology patients, and a definitive move away from non-evidence-based dietary supplements.
Fig. 1: Legend for graphical abstract: 2025 ESC/EAS Dyslipidaemia Guidelines. The 2025 ESC/EAS Guidelines mark a paradigm shift in cardiovascular risk management, championing a “sooner, lower, better” approach. These evidence-based updates provide clinicians with robust tools for personalized cardiovascular risk reduction across diverse patient populations
Refined risk estimation: the foundation of treatment
A fundamental shift is the replacement of the old SCORE algorithm with SCORE2 (ages 40–69) and SCORE2-OP (ages 70–89).1 This is a critical advancement as it estimates the 10-year risk of both fatal and non-fatal CV events, extending sophisticated risk assessment to the elderly population. The new risk categories (low, moderate, high, very high) are based on doubled SCORE2 thresholds, reminding us that these are pragmatic cut-offs on a continuous risk spectrum.
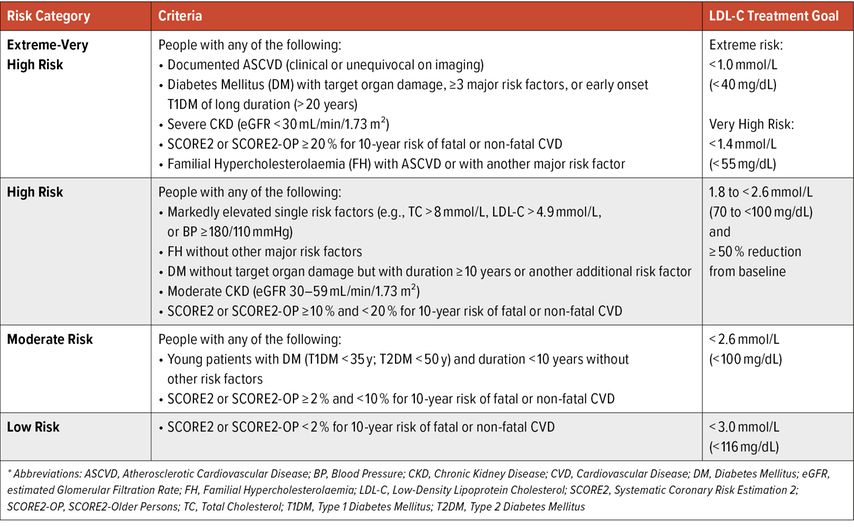
Impactful is also the enhanced role of risk modifiers in moderate-risk patients. The presence of subclinical atherosclerosis, as detected by imaging (e.g., carotid plaque) or an elevated coronary artery calcium (CAC) score, should be considered a risk-enhancing factor that can modify risk assessment in adults estimated to be at moderate risk or in those near treatment thresholds based on the SCORE2/SCORE2-OP algorithms.1 An important caveat is that the interpretation of a CAC score must be approached with caution in patients already on statin therapy. Statins promote plaque stabilisation, which can manifest as a decrease in lipid-rich plaque and a potential increase in calcification; therefore, a rising CAC score in this context may not indicate disease progression but rather a treatment effect (Table 1).
Table 1: Cardiovascular Risk Categories (based on SCORE2/SCORE2-OP) - updated of table 4 from the 2019 guidelines
The update also formally recognizes biomarkers, specifically elevated lipoprotein(a) [Lp(a)] >50mg/dL (105nmol/L) and high-sensitivity C-reactive protein (hs-CRP >2mg/L). These can and should be used to reclassify patients to a higher risk category, justifying more aggressive LDL-C targets and earlier intervention.1 The new recommendation highlights that assessment should be made in the broader context of the patient’s overall risk profile, which includes the following clinical and demographic risk modifiers: family history of premature CVD (men <55 years; women <60 years), high-risk ethnicity (e.g., South Asian), socioeconomic deprivation, major psychosocial stress, or psychiatric disorders, obesity and physical inactivity, history of premature menopause, pre-eclampsia, hypertensive disorders of pregnancy, chronic inflammatory disorders (e.g., rheumatoid arthritis), HIV infection, or obstructive sleep apnoea.1
Intensified LDL-C goals and expanded therapeutic arsenal
The LDL-C goals remain stratified by risk, but the context for setting them is now sharper. The emphasis on achieving a ≥50% reduction from baseline alongside absolute targets is reinforced across all categories, highlighting the importance of both relative intensity and absolute goal fulfilment.
The landscape of available therapeutics has expanded significantly
Based on the 2025 Focused Update, LDL-C goals remain risk-stratified, with reinforced emphasis on achieving both a ≥50% reduction from baseline and absolute targets.1
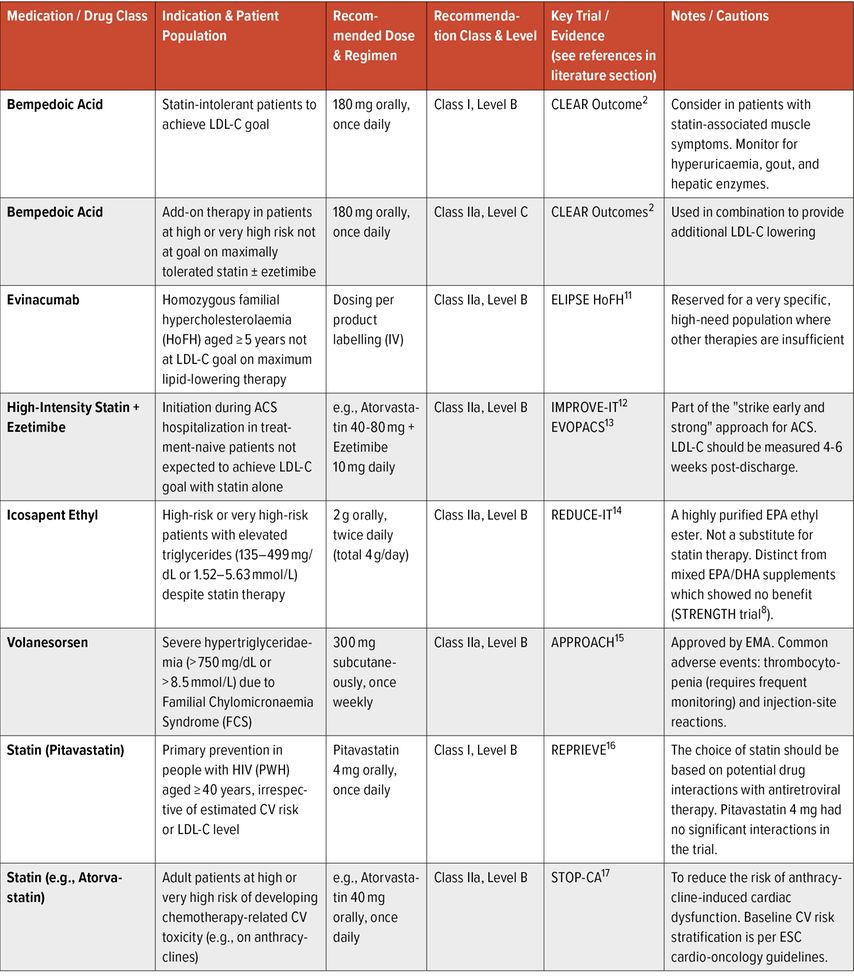
Key therapeutic updates include a Class I recommendation for bempedoic acid in statin-intolerant patients, supported by the CLEAR Outcomes trial demonstrating 13% MACE reduction despite risks of hepatic enzyme elevation, hyperuricaemia, gout, and renal impairment (Table 2).2
Table 2: New and updated Pharmacological Treatment Recommendations from the 2025 ESC/EAS Focused Update1
For combination therapy, non-statin agents (ezetimibe, PCSK9 mAbs, or bempedoic acid) are recommended (Class I, Level A) added to maximally tolerated statins, with selection based on required LDL-C lowering, preference, and cost (Table 2).
Evinacumab receives a Class IIa recommendation for homozygous FH patients ≥5 years, reducing LDL-C by nearly 50%1 (Table 2).
Inclisiran remains under investigation. Clinicians should individualise therapy, monitor LDL-C 4–6 weeks post-initiation, and refer to efficacy data (Table 1).
Acute coronary syndromes: mandating in-hospital, intensive intervention
The update addresses a critical care gap: the high early recurrent risk post-ACS. Evidence from trials like HUYGEN,3 PACMAN-AMI,4 and SWEDEHEART5 confirms that early, intensive LDL-C lowering is safe and effective, championing the “the sooner, the lower, the better” paradigm. The guidelines now mandate proactive, in-hospital initiation of intensive lipid-lowering therapy for all ACS patients (Class I), involving immediate high-intensity statin therapy and the seamless addition of ezetimibe if needed to achieve goal, with all therapy intensified before discharge to maximize risk reduction during the highest-risk post-event period.1
Personalized strategies for specific populations
The 2025 update introduces key recommendations for specific populations: people with HIV (PWH) aged ≥40 should receive pitavastatin for primary prevention (35% MACE reduction per REPRIEVE);6 atorvastatin is recommended for lymphoma patients on anthracyclines to reduce cardiotoxicity (STOP-CA);7 high-dose icosapent ethyl (not other omega-3 mixes) is advised for high-risk patients with elevated triglycerides (REDUCE-IT);8 and volanesorsen is indicated for familial chylomicronaemia syndrome (FCS) to lower triglycerides and pancreatitis risk.1
A definitive stance on dietary supplements
In a clear departure from past ambiguity, the update issues a definitive Class III recommendation (i.e., not recommended) against using dietary supplements—including fish oil (except high-dose IPE in specific settings), red yeast rice, and plant sterols—for ASCVD risk reduction. This position, reinforced by trials like SPORT9 and OMEMI10 and EU regulatory actions, emphasizes evidence-based dietary patterns over unproven supplements.
Take-home messages
Towards personalised, early and proactive intensive lipid-lowering management
The 2025 Focused Update endorses a decisive shift in CV prevention, utilising new risk tools (SCORE2, modifiers) for precise stratification, and biomarkers to reclassify risk. The update recommends to initiate intensive lipid lowering treatment early (especially post-ACS), and provides key treatment recommendations for specific populations (for HIV, cancer, statin intolerance). Finally, it recommends against the use of non-evidence-based dietary supplements. The core directive is to personalise care and act earlier, adapting a more intensive lipid-lowering management to reduce ASCVD burden.
Literature:
1 Mach F et al.: 2025 Focused Update of the 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Developed by the task force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J 2025; doi: https://doi.org/10.1093/eurheartj/ehaf190 2 Nissen SE et al.: Bempedoic acid and cardiovascular outcomes in statin-intolerant patients. N Engl J Med 2023; 388(15): 1353-64 3 Nicholls SJ et al.: Effect of evolocumab on coronary plaque phenotype and burden in statin-treated patients following myocardial infarction. JACC Cardiovasc Imaging 2022; 15(7): 1308-21 4 Raber L et al.: Effect of alirocumab added to high-intensity statin therapy on coronary atherosclerosis in patients with acute myocardial infarction: The PACMAN-AMI randomized clinical trial. JAMA 2022; 327(18): 1771-81 5 Schubert J et al.: Intensive early and sustained lowering of non-high-density lipoprotein cholesterol after myocardial infarction and prognosis: the SWEDEHEART registry. Eur Heart J 2024; 45(3): 4204-15 6 Grinspoon SK et al.: Pitavastatin to prevent cardiovascular disease in HIV infection. N Engl J Med 2023; 389(8): 687-99 7 Neilan TG et al.: Atorvastatin for anthracycline-associated cardiac dysfunction: the STOP-CA randomized clinical trial. JAMA 2023; 330(6): 528-36 8 Bhatt DL et al.: Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med 2019; 380(1): 11-22 9 Laffin LJ et al.: Comparative effects of low-dose rosuvastatin, placebo, and dietary supplements on lipids and inflammatory biomarkers. J Am Coll Cardiol 2023; 81(1): 1-12 10 Kalstad AA et al.: Effects of n-3 fatty acid supplements in elderly patients after myocardial infarction: a randomized, controlled trial. Circulation 2021; 143(6): 528-39 11 Raal FJ et al.: Evinacumab for homozygous familial hypercholesterolemia. N Engl J Med 2020; 383: 711-2 12 Cannon CP et al.: Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med 2015; 372: 2387-97 13 Koskinas KC et al.: Evolocumab for early reduction of LDL cholesterol levels in patients with acute coronary syndromes (EVOPACS). J Am Coll Cardiol 2019; 74: 2452-62 14 Bhatt DL et al.: Cardiovascular risk reduction with icosapent ethyl for hypertriglyceridemia. N Engl J Med 2019; 380: 11-22 15 Witztum JL et al.: Volanesorsen and triglyceride levels in familial chylomicronemia syndrome. N Engl J Med 2019; 381: 531-42 16 Grinspoon SK et al.: Pitavastatin to prevent cardiovascular disease in HIV infection. N Engl J Med 2023; 389: 687-99 17 Neilan TG et al.: Atorvastatin for anthracycline-associated cardiac dysfunction: the STOP-CA randomized clinical trial. JAMA 2023; 330: 528-36
Das könnte Sie auch interessieren:
Stellenwert der nuklearmedizinischen Bildgebung zur Überwachung des Therapieverlaufs bei kardialer Amyloidose
Nuklearmedizinische Bildgebungsverfahren mit Amyloid-affinen Tracern haben sich als nichtinvasiver Goldstandard für die Diagnostik der Transthyretin-Amyloid-Kardiomyopathie (ATTR-CM) ...
ESC-Guideline zur Behandlung von Herzvitien bei Erwachsenen
Kinder, die mit kongenitalen Herzvitien geboren werden, erreichen mittlerweile zu mehr 90% das Erwachsenenalter. Mit dem Update ihrer Leitlinie zum Management kongenitaler Vitien bei ...
ESC gibt umfassende Empfehlung für den Sport
Seit wenigen Tagen ist die erste Leitlinie der ESC zu den Themen Sportkardiologie und Training für Patienten mit kardiovaskulären Erkrankungen verfügbar. Sie empfiehlt Training für ...