Versatile use of picosecond lasers
Autthors:
cand. med. Stella Vocke1
Jitaraphol Potiwihok, M.D.2
Dr. med. C. Bettina Rümmelein3
1 University of Zurich, Switzerland
2 Chulabhorn International College of Medicine Thammasat University, Pathum Thani, Thailand
3 Hautwerk, Zurich, Switzerland
E-Mail: klinik@hautwerk.ch
Since the development of picosecond lasers in 2012 for the optimization of tattoo removal treatments, many further indications have been found. This article gives an overview of the history of rapid development over the past 13 years and an outlook on the future of picosecond lasers.
Keypoints
-
Picosecond lasers represent a breakthrough evolution in dermatologic laser technology, offering ultrashort photomechanical pulses that provide precise pigment targeting with less collateral damage —building upon decades of innovation since the era of Q-switched lasers.
-
Picosecond lasers are now well-established for tattoo removal and benign pigmented lesions, and have gained increasing evidence for use in melasma, skin rejuvenation, and acne scar revision, especially in darker skin types due to their favorable safety profile.
-
Next-generation picosecond systems with shorter pulse durations, expanded wavelengths, and advanced optical components are poised to further refine treatment precision, enabling safer, more personalized therapies across a broader spectrum of dermatologic concerns.
Picosecond lasers are ultrashort-pulse laser systems characterized by pulse durations in the order of 10–12 seconds. This extremely short pulse width, significantly shorter than the nanosecond (10–9s) pulses of earlier Q-switched lasers, allows picosecond devices to deliver energy with very high peak power in a brief timeframe.1 The mechanism of action is predominantly photomechanical (photoacoustic) rather than photothermal; the rapid, high-intensity pulses shatter target chromophores (such as tattoo ink or melanin pigment) into microscopic particles via acoustic shock waves, with minimal heat diffusion to surrounding tissue.1
By confining laser energy deposition to the target’s thermal relaxation time, picosecond lasers achieve highly selective destruction of pigment while sparing normal skin structures.2 In practical terms, this means greater precision in targeting unwanted pigmentation and less damage to adjacent tissue compared to traditional nanosecond lasers.3
In dermatology, these attributes translate into several significant clinical advantages. Picosecond lasers have demonstrated superior efficacy in tattoo removal and pigmented lesion treatment. Studies have shown that picosecond-domain pulses can achieve equal or higher clearance of tattoo ink in fewer treatment sessions than nanosecond Q-switched lasers, with a lower risk of adverse effects.3 Resistant tattoo colors (especially blues and greens) can be more effectively cleared with picosecond devices.4 Likewise, benign pigmented lesions such as nevus of Ota, melasma, and lentigines have been treated with picosecond lasers, although careful settings are needed to minimize post-inflammatory hyperpigmentation (PIH) in darker skin types.5
Beyond pigment removal, the picosecond platform has proven versatile for skin rejuvenation. Using special fractional diffractive lens arrays, picosecond lasers can create laser-induced optical breakdown (LIOB) microinjuries in the epidermis and dermis, stimulating new collagen and elastin production for improvement of acne scars, photoaged skin, and fine wrinkles.6 Clinically, dermatologists have observed that picosecond treatments for atrophic acne scars can produce comparable improvement to traditional fractional ablative lasers but with reduced downtime and lower risk of complications, thanks to the picosecond’s low residual thermal damage profile.6
As a recent review summarized, the advent of picosecond pulse technology represents a “breakthrough innovation in laser technology,” expanding the scope of laser treatments with encouraging results and a low incidence of adverse effects across a variety of dermatologic applications.1
History of picosecond laser
The development of picosecond laser technology in dermatology is rooted in decades of laser innovation. The first working laser was demonstrated by Theodore Maiman in 1960 using a ruby crystal medium (694nm), and shortly thereafter, dermatologic pioneers like Leon Goldman began experimenting with lasers for pigmented lesions.7 Early laser systems were continuous-wave or long-pulsed, often causing significant nonspecific thermal injury to skin.
A major turning point came in 1983 with the introduction of the theory of selective photothermolysis by Anderson and Parrish.2 This principle held that optimal targeting of a specific chromophore (such as tattoo ink or melanin) could be achieved by using a pulse duration shorter than the thermal relaxation time of the target, thereby confining heat to the target and sparing surrounding tissue. Selective photothermolysis laid the scientific groundwork for Q-switched lasers, which deliver nanosecond-scale pulses and became the standard for tattoo removal and pigment treatments through the late 20th century. Q-switched ruby, alexandrite, and Nd:YAG lasers (with pulse durations in the 5–100 ns range) were widely adopted in the 1980s and 1990s, dramatically improving outcomes compared to earlier continuous lasers.8 However, some tattoo inks remained difficult to eradicate, and excessive thermal injury could still occur.
This prompted the development of even shorter pulse durations. The concept of producing picosecond pulses was enabled by advances in mode-locking techniques and laser media during the late 20th century.1 By the mid-1990s, experimental lasers were capable of generating picosecond-range pulses, and around 1998, researchers reported that experimental picosecond lasers could clear tattoo ink more efficiently than nanosecond devices, causing greater fragmentation with less collateral damage.9 These trials confirmed theoretical advantages, but clinical deployment required further refinement in energy delivery and stability.
A pivotal moment came in 2012, when the U.S. FDA granted 510(k) clearance for the first picosecond laser for aesthetic use—the 755nm Alexandrite system (PicoSure®, Cynosure Inc., Westford, MA, USA). This device demonstrated faster and more complete tattoo clearance, especially for difficult colors like green and blue.4 Other wavelengths soon followed, including 532 and 1064nm from Nd:YAG sources, broadening clinical applications. Around 2014–2015, fractional picosecond handpieces (e.g., diffractive lens array, microlens array [MLA]) were introduced, allowing picosecond lasers to target the dermis non-ablatively, stimulating collagen remodeling without significant thermal injury.6 This innovation greatly expanded applications to include acne scars, wrinkles, and skin texture improvement.
Today, picosecond lasers are widely used in dermatology as highly precise and safe tools. Their evolution – from ruby lasers to nanosecond Q-switched devices, and finally to picosecond systems – illustrates the continuous refinement in laser medicine, driven by a desire for selective targeting and reduced downtime.1
Indications
Picosecond laser technology was initially introduced to optimize tattoo removal, and it has since been applied to a broadening range of dermatological conditions. A comprehensive systematic review published in 2020 in Lasers in Surgery and Medicine evaluated over 200 studies and proposed evidence-based guidelines for clinical picosecond laser use.10 According to this review, picosecond lasers have level 1 evidence support for tattoo removal and varying levels of evidence (levels 1–4) for treating benign pigmented lesions, along with level 2 evidence for skin rejuvenation and melasma, and level 2–3 evidence for scar revision.
Tattoo removal
Tattoo removal remains the original and most well-established indication for picosecond lasers. Compared to traditional nanosecond Q-switched devices, picosecond 755nm alexandrite and 1064nm Nd:YAG lasers fragment tattoo ink more efficiently, achieving faster clearance in fewer sessions. For example, a 2024 prospective study in 20 Fitzpatrick IV patients observed ∼60% clearance of black tattoos after two picosecond 1064nm laser sessions, with no scarring or pigmentary loss.11 Typical treatment intervals are 6–8 weeks. Transient erythema, edema, and pinpoint bleeding are common side effects, but the risk of lasting hypopigmentation or textural change is low.12 Today, picosecond lasers are considered the gold standard for laser tattoo removal (level 1a evidence), reflecting strong consensus on its superior efficacy and safety compared to older Q-switched methods.
Recent techniques involve multiple-pass treatments (R0/R20 methods) with perfluorodecalin patches, significantly accelerating tattoo pigment clearance and reducing overall treatment sessions without increased skin damage.13
Melasma
Several studies continue to evaluate the nuanced role of picosecond lasers in the management of melasma. A 2023 meta-analysis of six randomized controlled trials (RCTs), primarily in Asian populations, demonstrated that picosecond lasers — particularly at the 1064nm wavelength (Nd:YAG) — significantly reduced modified Melasma Area and Severity Index (mMASI) scores without serious adverse effects. Subgroup analysis confirmed that 1064nm picosecond lasers were both safe and effective for melasma treatment, while the 755nm alexandrite picosecond laser showed no significant advantage over topical depigmenting agents and was associated with a higher incidence of PIH.14
To improve outcomes with the 755nm wavelength, recent investigations have explored combination regimens.15,16 In particular, the adjunctive use of topical tranexamic acid with a 755nm picosecond alexandrite laser has shown superior efficacy in reducing melasma severity and enhancing patient satisfaction compared to monotherapy or regimens involving hydroquinone. This combination also demonstrated a favorable safety profile with a reduced risk of PIH, an important consideration in patients with darker skin types.
The FDA’s 510(k) clearance of the PicoSure® Pro (Cynosure Inc., Westford, MA, USA) in March 2021 for melasma management reflects growing regulatory confidence in the safety of picosecond lasers for deeper pigmentary disorders and allows for on-label use.17 However, despite this advancement, the role of picosecond lasers remains adjunctive rather than primary. Melasma is a chronic, relapsing condition with multifactorial pathogenesis, and laser-induced inflammation can exacerbate pigmentation if not carefully controlled.
A 2020 systematic review classified picosecond laser treatment for melasma as level 2b evidence, underscoring the need for caution.10 Further, a 2022 systematic review and meta-analysis by Lai et al. found that while picosecond laser therapy led to some clinical improvement, it did not yield statistically significant reductions in MASI scores when compared to non-laser controls, reinforcing the conclusion that laser monotherapy provides modest and often inconsistent results.18
Given this, current consensus favors incorporating picosecond lasers into a multimodal treatment regimen, often including topical tyrosinase inhibitors, strict photoprotection, and adjunctive measures such as oral tranexamic acid or fractional thulium lasers. Patient education and expectation management remain critical, as melasma often requires long-term maintenance, and the risk of rebound hyperpigmentation persists.
Skin rejuvenation and pore reduction
Fractional picosecond lasers have gained popularity for skin rejuvenation and pore tightening, known as a “lunchtime procedure” due to minimal downtime. By using intradermal laser-induced cavitation (LIC) and LIOB, skin remodeling is encouraged and collagen production is stimulated (evidence level 2a).6 A 2025 study in a Vietnamese cohort supports current indications for picosecond lasers by showing their safe and effective use in melanin-rich skin for facial rejuvenation. The fractional 1064nm Nd:YAG picosecond laser demonstrated significant improvement in wrinkles, pigmentation, and skin texture as early as one-month post-treatment and sustained significant improvements at three months.19
Complementing these findings, a 2024 split-face RCT comparing the fractional 1064nm picosecond laser with a 1565nm nonablative fractional laser reported equivalent pore size reduction and patient satisfaction after three sessions but notably less pain with the picosecond treatment. There was no significant difference in PIH occurrence.20 Clinical experience suggests that fractional picosecond treatments can achieve moderate improvements in skin tone and texture, although results may not be as dramatic as with aggressive ablative lasers. One advantage observed is an improved side-effect profile compared to traditional non-ablative fractional lasers.21 Specifically, picosecond fractional lasers tend to cause less PIH and less procedural pain, which is especially important for patients with darker skin types who are at higher risk of pigmentary side effects. The downtime is minimal — often limited to mild redness for a day or two and pinpoint bleeding. This contrasts with some older resurfacing lasers that may induce more prolonged erythema or swelling.
Atrophic acne scars
Significant advancements occurred in treating atrophic acne scars with fractional picosecond lasers. A 2023 split-face RCT comparing fractional 1064nm Nd:YAG picosecond laser (MLA) with 2940nm ablative fractional Er:YAG laser showed comparable scar improvement based on ECCA and IGA scores in Asian patients. The picosecond laser demonstrated lower pain, shorter recovery periods, as measured by the duration of crust shed and edema, and significantly lower PIH incidence.22
Moreover, a 2023 pilot study established the safety of using picosecond lasers concurrently with oral isotretinoin, suggesting the feasibility of early acne scar intervention even during ongoing low-dosed isotretinoin therapy without increased scarring risk. It was a split-face study, with one randomly chosen side of the face being treated with fractional picosecond 106nm Nd:YAG Laser and the other side being left untreated as control. There was a significant improvement in the ECCA score as seen on the treated side, with no adverse effects having been reported.23
Benign pigmented lesions
Newer advances include the clinical introduction of the 730nm Ti:Sapphire picosecond laser, FDA-commercialized around 2020 and initially validated for multicolored tattoo removal. It delivers pulse durations as short as 240–250ps — among the shortest in the picosecond domain at that time. Since then, multiple studies have demonstrated its safety and efficacy in treating a broad spectrum of benign pigmentary disorders, including lentigines, freckles, café-au-lait macules (CALM), melasma, and nevus of Ota, across various skin types with minimal adverse effects.24,25 A 2025 large-scale Asian study further expanded its clinical indications, reporting significantly greater clearance (∼88%) and patient satisfaction (∼94%) in acquired dermal melanocytosis (ADM) compared to traditional 1064nm lasers, positioning the 730nm Ti:Sapphire picosecond laser as a highly effective modality for pigment-targeted treatment in melanin-rich skin.26
Nevus of Ota
Picosecond lasers are considered a first-line treatment for nevus of Ota, supported by high-level evidence (level 1b). Multiple studies have reported significant pigment clearance in these bluish dermal patches. For instance, a large retrospective study in 2024 treated 305 pediatric nevus of Ota patients with a 755nm picosecond alexandrite laser, achieving on average ∼79% clearance after about two sessions.30 The majority of patients had excellent responses, and the treatment was deemed safe and effective, even in children. This underscores that picosecond laser is highly effective for nevus of Ota, with better outcomes seen when treatment is started at younger ages and for darker lesions.27
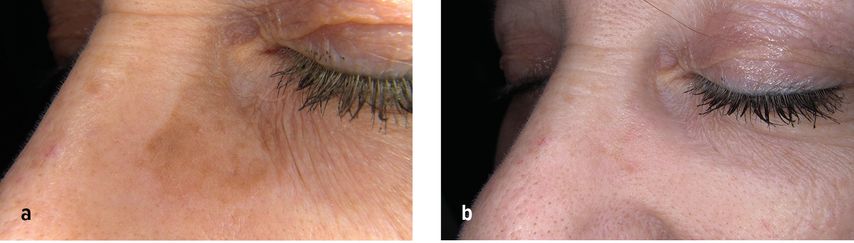
Abb. 2a/b: Before and after one treatment with a picosecond laser (one month later)
Hori’s macules
These bluish-brown patches on the cheeks, which are common in Asian skin, are closely related to nevus of Ota. Picosecond lasers also serve as a first-line therapy for Hori’s macules, with outcomes similar to the treatment of nevi of Ota. Patients typically achieve significant fading of the macules after a series of picosecond laser sessions.
Solar lentigines
Studies show high clearance rates and patient satisfaction for lentigines treated with picosecond pulses (evidence level 2b). However, the advantage of picosecond over nanosecond Q-switched lasers in lentigines is less clear. Some comparative data suggest that both picosecond and nanosecond lasers achieve similar outcomes for these superficial brown spots.10 In practice, picosecond lasers remove lentigines with minimal downtime, but clear superiority in efficacy over older Q-switched devices has not been definitively proven for this indication.
Freckles
Likewise, freckles have been treated with picosecond lasers with good success (level 2b evidence). A 2024 pilot study using 730 nm showed substantial clearance (∼74.5%) in twelve Chinese patients after just one session, high aesthetic improvement scores, minimal pain, and negligible adverse effects.28 As with lentigines, the efficacy is comparable to nanosecond laser treatments, so picosecond lasers are a safe and effective option, but not necessarily dramatically better than traditional methods in terms of final outcome. They do, however, offer the benefit of shorter pulse duration which might reduce collateral damage and potentially lower the risk of post-inflammatory changes in susceptible individuals.
Café-au-lait macules (CALM)
These congenital light-brown patches have been treated with picosecond lasers with mixed results. The evidence is relatively low, consisting of small case series and anecdotal reports. Some patients experience partial fading of café-au-lait spots with picosecond laser sessions, but complete clearance is variable, and recurrence can occur. Due to the patches’ epidermal nature and potential recurrence, treatment of CALMs remains challenging, and evidence for picosecond laser efficacy is not robust in this area. Picosecond lasers are used off-label with cautious optimism in select cases.
Technological innovations
Emerging technologies introduced shorter pulse durations (∼250ps) and higher peak power (up to 2 GW), significantly enhancing pigment fragmentation efficiency with reduced thermal side effects.29 Newer picosecond laser platforms incorporate multiple wavelengths (532nm, 595nm, 660nm, 1064nm) and dual pulse durations (nano- and picosecond modes), providing versatility and improved treatment outcomes across diverse indications.29
Additionally, advanced optical elements like diffractive optical elements (DOE) and MLAs have been further refined, allowing customized depth and energy distribution for various skin conditions, from deep acne scars to superficial pigmentary issues.17
Conclusion
Technical development of picosecond lasers is ongoing, with further advancements anticipated in the near future. The possible applications of picosecond lasers are extremely diverse, and they therefore represent a sensible extension of the classic laser therapy spectrum. In particular, they offer a safe and effective treatment option for patients with skin of color – populations historically more vulnerable to PIH. As evidence accumulates and indications expand, picosecond lasers are poised to play an increasingly central role in personalized, minimally invasive aesthetic and therapeutic dermatology.
Literature:
1 Torbeck RL et al.: Evolution of the picosecond laser: a review of the literature. Dermatol Surg 2019; 45(2): 183-94 2 Anderson RR, Parrish JA: Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science 1983; 220(4596): 524-7 3 Hsu VM et al.: The picosecond laser for tattoo removal. Lasers Med Sci 2016; 31(8): 1733-7 4 Jakus J, Kailas A: Picosecond lasers: a new and emerging therapy for skin of color, minocycline-induced pigmentation, and tattoo removal. J Clin Aesthet Dermatol 2017; 10(3): 14-5 5 Forbat E, Al-Niaimi F: The use of picosecond lasers beyond tattoos. J Cosmet Laser Ther 2016; 18(6): 345-7 6 Zhou Y et al.: An update on fractional picosecond laser treatment: histology and clinical applications. Lasers Med Sci 2023; 38(1): 45 7Gianfaldoni S et al.: An Overview of Laser in Dermatology: The Past, the Present and … the Future (?). Open Access Maced J Med Sci 2017; 526-308 Ross V et al.: Comparison of responses of tattoos to picosecond and nanosecond Q-switched neodymium: YAG lasers. Arch Dermatol 1998; 134(2): 167-719Alabdulrazzaq H et al.: Clearance of yellow tattoo ink with a 532-nm picosecond laser. Lasers Surg Med 2015; 47(4): 285-810 Wu DC et al.: A systematic review of picosecond laser in dermatology: evidence and recommendations. Lasers Surg Med 2021; 53(1): 9-49 11 Ismail MA et al.: Removal of black tattoos by picosecond Q-switched Nd-YAG laser in the middle eastern skin type IV: prospective study. Lasers Med Sci 2024; 39(1): 214 12 Odermatt H, Rümmelein B: Einsatzmöglichkeiten von Pikosekundenlasern. Leading Opin Dermatol Plast Chir 2023; 2: 32-4 13 Vangipuram R et al.: Perfluorodecalin-infused patch in picosecond and Q-switched laser-assisted tattoo removal: safety in Fitzpatrick IV-VI skin types. Lasers Surg Med 2019; 51(1): 23-6 14 Feng J et al.: Efficacy and safety of picosecond laser for the treatment of melasma: a systematic review and meta-analysis. Lasers Med Sci 2023; 38(1): 84 15Zhou N et al.: Safety and efficacy of a picosecond 755-nm alexandrite laser combined with topical tranexamic acid in the treatment of melasma. J Cosmetic Dermatol2024; 23(11): 3579-8416 Pulumati A et al.: The role of 755-nm alexandrite picosecond laser in melasma management. Arch Dermatol Res 2023; 316(1): 60 17 Cynosure. PicoSure Pro Product Manual. Westford, MA: Cynosure Inc.; 2022 18 Lai D et al.: Laser therapy in the treatment of melasma: a systematic review and meta-analysis. Lasers Med Sci 2022; 37(4): 2099-110 19 Le TVT et al.: Fractional 1064 nm Nd:YAG picosecond laser for Asian skin rejuvenation: clinical efficacy and the role of photoprotective behaviours. Lasers Med Sci 2025; 40(1): 209 20 Liu X et al.: Comparison of the 1064-nm picosecond laser with fractionated microlens array and 1565-nm non-ablative fractional laser for the treatment of enlarged pores: a randomized, split-face, controlled trial. Lasers Med Sci 2024; 39(1): 80 21 Li J et al.: Fractional picosecond laser for atrophic acne scars: a meta-analysis. J Cosmet Dermatol 2023; 22(8): 2205-17 22Dai R et al.: Comparison of 1064-nm Nd:YAG picosecond laser using fractional micro-lens array vs. ablative fractional 2940-nm Er:YAG laser for the treatment of atrophic acne scar in Asians: a 20-week prospective, randomized, split-face, controlled pilot study. Front Med (Lausanne) 2023; 10: 124883123 Xue H et al.: Early acne scar intervention with 1064 nm picosecond laser in patients receiving oral isotretinoin: a randomized split-face controlled pilot study. Lasers Med Sci 2023; 38(1): 40 24 Han R et al.: Efficacy and safety of 730-nm picosecond laser for the treatment of acquired bilateral nevus of Ota-like macules. Dermatol Surg 2025; 51(5): 485-9 25 Lipp MB et al.: Safety and efficacy of a novel 730 nm picosecond titanium sapphire laser for the treatment of benign pigmented lesions. Lasers Surg Med 2021; 53(4): 429-34 26Takaya K, Kazuo K: Comparison of the Efficacy of 1064- and 730-nm Picosecond Lasers for Acquired Dermal Melanocytosis. J Cosmet Dermatol 2025; 24(3): e7012327 Zhao W et al.: Picosecond alexandrite laser treatment of nevus of Ota in children. Lasers Surg Med 2024; 56(5): 437-45 28Huang Y et al.: Successful Treatment of Freckles Using a 730-nm Picosecond Laser: A Prospective Study. Clin Cosmet Investig Dermatol 2024; 17: 3027-3229 Ryu H et al.: Development of 250 picosecond Nd:YAG laser for dermatologic applications in Republic of Korea: development report. Med Lasers 2022; 11(4): 229-35
Das könnte Sie auch interessieren:
Gesichtsischämie und vaskuläre Komplikationen nach Filler-Injektion
Vaskuläre Komplikationen nach ästhetischen Filler-Injektionen stellen eine ernsthafte, aber seltene Herausforderung dar. Wir berichten über den Fall einer Patientin mit Gesichtsischämie ...
Patientenerlebnis als strategischer Erfolgsfaktor
Ästhetische Praxen unterscheiden sich nicht nur durch Behandlungen, sondern auch durch das Erlebnis. Wer digitale Präsenz, Ambiente, Konsultation und Nachsorge konsequent gestaltet, ...
Rajeunissement intime féminin: une solution innovante avec l’acide hyaluronique
Le bien-être intime féminin est un enjeu majeur de santé et de qualité de vie. La sécheresse vaginale, l’atrophie vulvo-vaginale et les douleurs lors des rapports affectent de nombreuses ...