Evidence-based long-term results after reverse shoulder arthroplasty in 2020
Authors:
Dr. med. Barbara Wirth
Dr. sc. nat. Alex Marzel
Dr. med. Christian Jung Schulthess
Klinik Zürich
Correspondence:
E-Mail: barbara.wirth@kws.ch
Since Grammont’s development of a modern reverse shoulder arthroplasty system (RSA) in the 1980s, commercially available products have been on the market for almost 30 years. RSA has become a reliable treatment option for not only irreparable rotator cuff tears and cuff tear arthropathy (CTA) but several other indications. With perfection of technique and progress in implant design, there is still uncertainty concerning predictable long-term outcomes and complication rates.
Keypoints
-
Long-term results after RSA show a predictable and stable improvement of shoulder function and patient satisfaction.
-
Implant survivorship of 87% to 93% can be expected after 10 years.
-
Complication and revision rates are high in the long term.
-
In our registry, the main reasons for revision were infections, loosening and instability.
Today’s reverse shoulder prosthesis goes back to the original design by Grammont in the late 1980s. It is based on 2 biomechanical concepts: distalizing the humerus and medialization of the center of rotation (COR) at the glenoid component. This leads to higher pre-tension of the deltoid muscle, more functional strength and to a decrease of the mechanical torque at the glenoid component in order to withstand the increased stresses caused by the fixed fulcrum at site of the bone-prosthesis interface.1
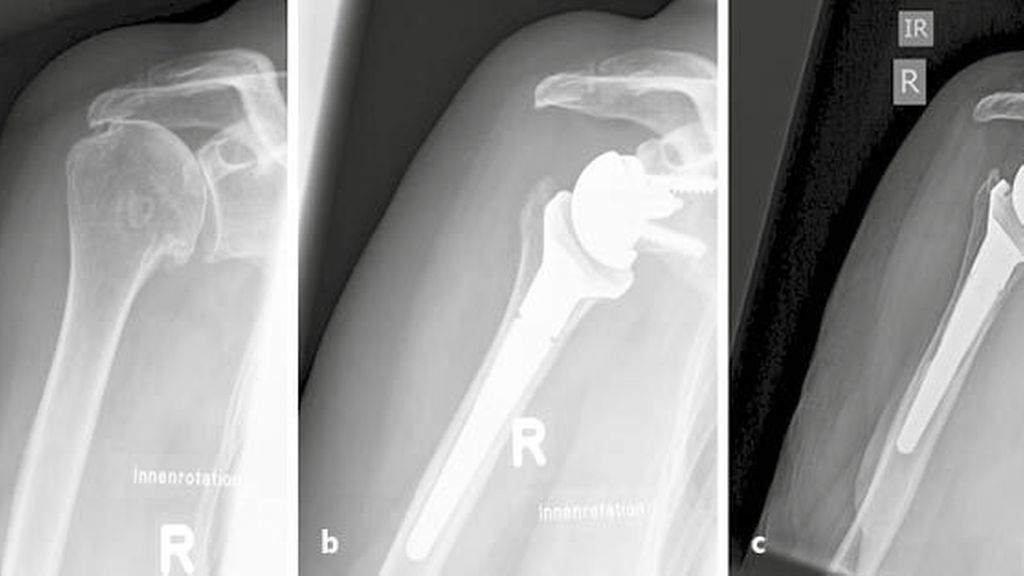
Over time there have been and still are ongoing changes and adjustments to the original biomechanical design, such as for example lateralization of the COR by bone graft or by lateralized baseplates/glenospheres, increased humeral off-set by alternating the neck-shaft angle or the cupdesign as well as inferior-eccentric glenosphere shape. Initially the reverse shoulder prosthesis was developed for arthropathies due to rotator cuff tears only (Fig.1).2
Fig. 1: a) preoperative CTA; b) 2 months postoperative after Lima Reverse (Lima Corporate); c) 10 years postoperative after Lima Reverse (Lima Corporate)
Over the last decade indications for RSA expanded due to reproducibly good results. This has led to an increase of RSA incidence3 with very promising short and midterm results.4 Yet it remains important to observe the long-term outcome. Complication rates after RSA are high5–7 and the term “complication” is widely used and not well defined.8 The purpose of this article is to display and compare the 10-years follow-up (FU) outcome of RSA of our own data with current evidence-based published results. Therefore, we analyzed our in-house shoulder arthroplasty registry data regarding functional results, patient-reported outcome and satisfaction, overall survival rate of the implant, revision rates and reasons for revision surgeries over ten years.
Analysis of the local Schulthess Shoulder Arthroplasty Registry (SAR)
Patient characteristics
Between March 2006 and October 2010, 462 eligible RSA operations were documented in the local Schulthess Shoulder Arthroplasty Registry (SAR). Mean age at baseline was 73.5 vears (SD 8.4), 74% were women. The type of implant used was Promos Reverse (Smith & Nephew) in 327 and Lima Reverse (Lima Corporate) in 135 shoulders.
Out of 462 cases that were potentially due for the 10 years follow-up, 115 were unfortunately reported as deceased. However, considering the age at baseline, it is likely that the number of deceased patients is underestimated. Overall, 167 were drop-outs, comprised of: 66 patients that were lost to follow-up, 10 who withdrew informed consent, 64 who could not attend the clinical examination or return the questionnaire because of health issues not related to the shoulder, and 27 patients, who were revised. Revision was defined as change or removal of at least one prosthesis component. 26 cases were not considered as drop-outs but their follow-up had to be postponed due to the Covid-19 situation.
Finally, 154 shoulders were available for analysis with a minimum of 10 years follow-up with either clinical examination or a questionnaire. Of those, 80 had both a questionnaire and clinical examination, 15 had only clinical examination and 59 had only a questionnaire.
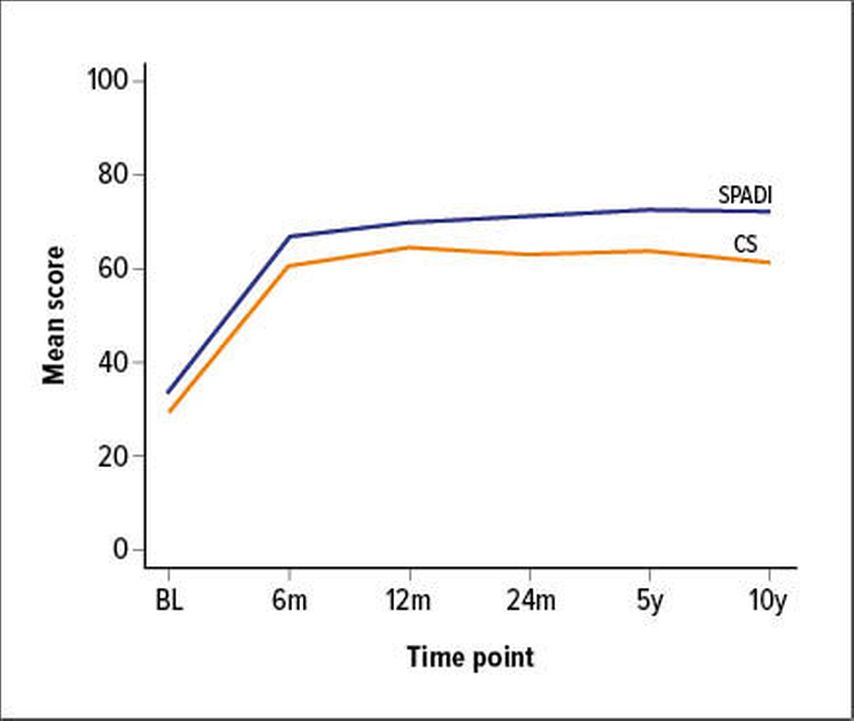
Functional outcomes
The functional and subjective outcome was recorded with the Constant and Murley Score (CS), Shoulder Pain and Disability Index (SPADI) and Subjective Shoulder Value (SSV). CS improved from a baseline mean of 29.2 (SD 13.3) to 63 (SD 16.3) at 2 years, 63.6 (SD 16.7) at 5 years and 61.3 (SD 16.7) at final 10 years (Fig.2).SPADI improved from baseline 33.6 (SD 18.8) to 71.2 (SD 21.8) at 2 years, 72.3 (SD 22.3) at 5 years and 72 (SD 22.1) at last 10 years FU. SSV was introduced to the registry at a later time point, therefore no baseline data is available. At 10 years FU it was reported at 73.8 (SD 19.6). To conclude, all recorded objective and subjective scores showed a significant and stable improvement over time, even 10 years after surgery.
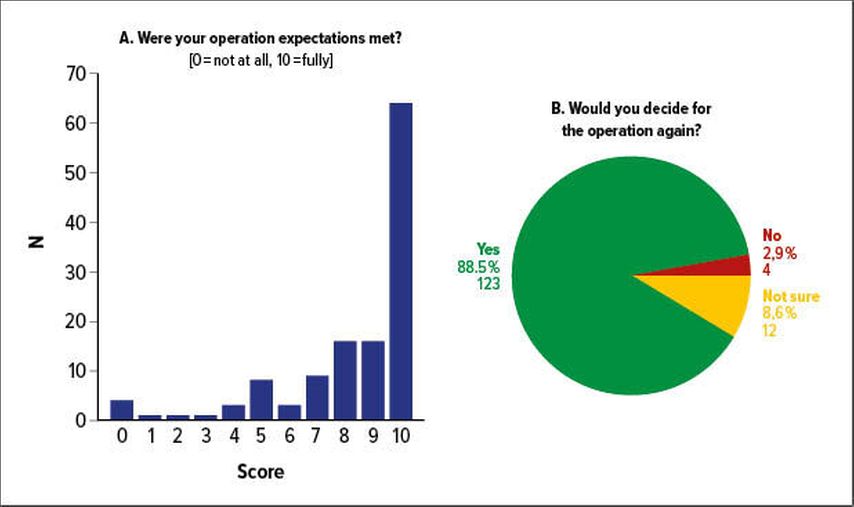
Patient long-term satisfaction
The patient-reported satisfaction rate was high: 63.5% stated that their expectations were met to an amount of 9 or 10 on the scale from 0 to 10 (Fig.3A). Postoperative expectation fulfillment remained stable over time with a mean of 8.3 at 2 years, 8.6 at 5 years and 8.3 at 10 years follow-up. When asked “If you were in the same situation as before your operation, would you decide to undergo this operation again with your current level of knowledge?” at 10 years follow-up 88.5% answered that they would do the surgery again, only 2.9% would not and the remaining were undecided (Fig.3B). In terms of quality of life, 87.3% reported a persistent improvement over the 10 years period compared to baseline.
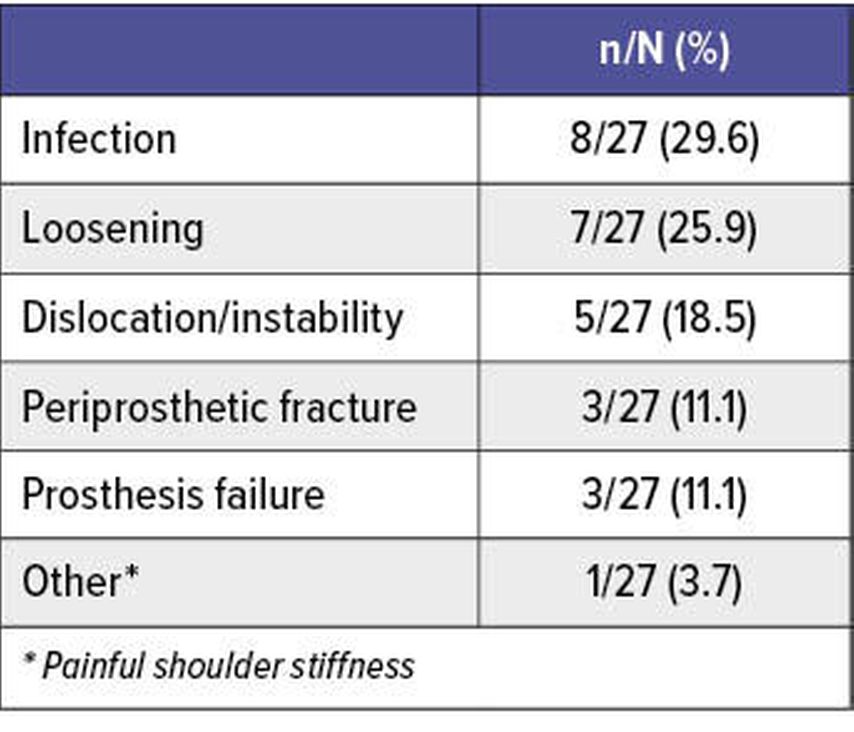
Implant survival
To our knowledge, 27 of the 462 initial RSA implants had to be revised which, when taking into account the individually contributed follow-up time, results in an overall prosthesis survival rate of 92% at 10 years. 13/27 cases are considered as RSA failure (defined according to Ernstbrunner et al.9 as explantation or transformation to hemiarthroplasty), 12 were replaced by hemiarthroplasty, 1 was removed and remained sine-sine. Further revision, defined as exchange of at least one prosthesis component, had to be performed in 14/27 cases. Overall, the two leading revision reasons were periprosthetic infections and loosening of the implant (Tab.1).
Evidence-based long-term results
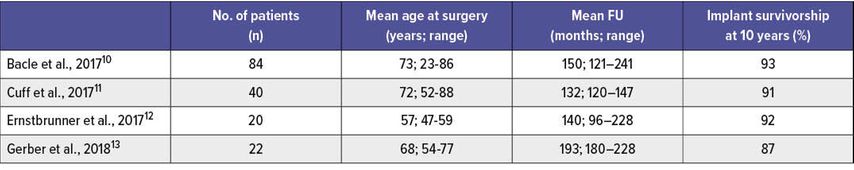
Nowadays several international working groups are following and monitoring their RSA patients continuously. While short- and mid-term results showed excellent results in terms of high patience satisfaction and low revision rate, there is still a lack of knowledge concerning long-term outcome of RSA. Only a few groups so far published RSA results with a mean FU of 10 years or longer (Tab.2).
It is important to be aware of the fact that reported results differ in terms of mean age at time of surgery and indication for surgery, making it somewhat difficult to compare the outcome results, revision rates and implant survivorship.
Irreparable tears or dysfunction of the rotator cuff with or without a joint destructing osteoarthritis (cuff tear arthropathy, CTA) are the most common indications for RSA. Ernstbrunner et al.9 reviewed the reported long-term results for patients with rotator cuff dysfunction with or without cuff tear arthropathy. After identifying a total cohort of 365 shoulders with a mean FU of 9.49 years (5–20), the analysis showed significantly improved shoulder function and clinical scores compared to preoperative status, even in the long run. The CS increased from 24 to 59 (p=0.004) and the SSV from 23% to 72% (p=0.049) thus very similar to our data.
A more thorough analysis of range of motion (ROM) revealed a gain of active anterior elevation from 66° to 127°, active abduction from 63° to 113° and statistically unchanged external rotation of 19° to 24° postop. Interestingly, no deterioration for CS and SSV over time was found in all studies that were following and observing their patients in a longitudinal way, including our cohort. Neither did they find any significant decrease of ROM over time after 5 and 10 years FU, as has been reported by other authors previously.14,15
Survivorship rates of implants at time of observation at 10 years FU ranged between 87–92% and 84–92% at 15 years FU.
Scapular notching grade III–IV was observed in 48% of all patients at 10 years FU. Its impact on implant survivorship as well as the reported complication/revision rates need to be monitored closely in the future. Favard et al.reported a complication rate of 18%,14 Ek et al. 38%,16 Ernstbrunner et al. as high as 39%.12
Bacle et al.10 and Cuff et al.11 reported on long-term results for a heterogenic cohort of indications, including rotator cuff tears, CTA, trauma sequela and revisions. Overall implant survivorship ranged between 91% and 93% at 10 years FU, which is in line with our data.
Trauma and trauma sequelae are another common indication for RSA. Long-term results after primary RSA in acute fracture situations are still scarce. Cazeneuve et al.17 reported a CS of 53 after a mean FU of 86 (12–204) months in 35 patients with a mean age of 75 (58–92) years. Revision rate was reported to be as high as 18%. Decroocq et al.18 reported similar results in 39 patients with a mean CS of 60 (8–81) after 83 (60–146) months.
RSA results for trauma sequela are in comparison with other indications less predictable, less successful and at higher risk for revision. The largest study (n=118) by Seeto et al.19 with a mean FU of 100 (60–185) months showed an CS of 53 (20–91) at final FU. Complications rates are as high as 73% for type 3 trauma sequela (classification according to Boileau et al.)20 and 94% in Type 4, resulting in a revision rate of 33% (Type 3) and 24% (Type 4). Previous surgery and loss of the tuberculum majus are negative predictors for a worse outcome, especially less ROM.
Ethics approval: This study is approved by the Ethical Committee of Canton Zürich (KEK-ZH-Nr. 2014-0483)
References:
1 Boileau P et al.: Neer award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 2006; 15(5): 527-40 2 Grammont PM, Baulot E: Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 1993; 16(1): 65-8 3 Kim SH et al.: Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 2011; 93(24): 2249-54 4 Schwyzer HK et al.: Short-term safety, function, and quality of life in patients treated with Univers Reverse prosthesis: a multicenter 2-year follow-up case series. J Shoulder Elbow Surg 2020; in press 5 Zumstein MA et al.: Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2011; 20(1): 146-57 6 Farshad M et al.: Revision of reversed total shoulder arthroplasty. Indications and outcome. BMC Musculoskeletal Disorders 2012; 13: 160 7 Fevang BT et al.: Risk factors for revision after shoulder arthroplasty: 1,825 shoulder arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop 2009; 80(1): 83-91 8 Glanzmann MC et al.: Re-intervention and revision rates following primary reverse total shoulder arthroplasty - review of a local shoulder arthroplasty registry. Int Orthop 2020; online ahead of print 9 Ernstbrunner L et al.: Long-term results of reverse total shoulder arthroplasty for rotator cuff dysfunction: a systematic review of longitudinal outcomes. J Shoulder Elbow Surg 2019; 28(4): 774-81 10 Bacle G et al.: Long-term outcomes of reverse total shoulder arthroplasty: a follow-up of a previous Study. J Bone Joint Surg Am 2017; 99(6): 454-61 11 Cuff DJ et al.: Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency: a concise follow-up, at a minimum of 10 years, of previous reports. J Bone Joint Surg Am 2017; 99(22): 1895-9 12 Ernstbrunner L et al.: Reverse total shoulder arthroplasty for massive, irreparable rotator cuff tears before the age of 60 years: long-term results. J Bone Joint Surg Am 2017; 99(20): 1721-9 13 Gerber C et al.: Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elbow Surg 2018; 27(5): 831-8 14 Favard L et al.: Reverse prostheses in arthropathies with cuff tear: are survivorship and function maintained over time? Clin Orthop Relat Res 2011; 469(9): 2469-75 15 Guery J et al.: Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 2006; 88(8): 1742-7 16 Ek ET et al.: Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg 2013; 22(9): 1199-208 17 Cazeneuve JF, Cristofari DJ: Long term functionaloutcome following reverse shoulder arthroplasty in the elderly. Orthop Traumatol Surg Res 2011; 97(6): 583-9 18 Decroocq L et al.: Long-term results of RSA for acute fractures. In: Boileau P et al. (ed.): Shoulder concepts: reverse shoulder arthroplasty. Montpellier: Sauramps Medical; 2016: 107-8 19 Seeto B et al.: Reverse shoulder arthroplasty for fracture sequelae: a minimum 5 year follow-up In: Boileau P et al. (ed.): Shoulder concepts: reverse shoulder arthroplasty. Montpellier: Sauramps Medical; 2016: 109-20 20 Boileau P et al.: Shoulder arthroplasty for the treatment of the sequelae of fractures of the proximal humerus. J Shoulder Elbow Surg 2001; 10(4): 299-308
Das könnte Sie auch interessieren:
Periphere Nervenkompressionssyndrome der oberen Extremität
Periphere Nervenkompressionssysteme der oberen Extremitäten sind verhältnismäßig häufig, insbesondere der Nervus medianus und der Nervus ulnaris sind oft im Bereich des Hand- bzw. ...
Konservative Behandlungsmöglichkeiten bei peripheren Nervenläsionen
Eine periphere Nervenläsion erfordert nicht nur eine Dekompression, Naht oder Rekonstruktion. Um Gelenke beweglich zu erhalten, eine Atrophie der Muskulatur zu verhindern und die ...
Bildgebende Diagnostik des peripheren Nervensystems
Die komplexen Nerventopografien machen die Nervenbildgebung zu einer fordernden Aufgabe, die allerdings eine wichtige Rolle dabei spielt, eine funktionelle Wiederherstellung der ...