From traditional methods to innovative treatments
Authors:
cand. med. Loraine Marino
Dr. med. C. Bettina Rümmelein
Hautwerk AG, Zurich
E-Mail: klinik@hautwerk.ch
Vielen Dank für Ihr Interesse!
Einige Inhalte sind aufgrund rechtlicher Bestimmungen nur für registrierte Nutzer bzw. medizinisches Fachpersonal zugänglich.
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
The pathogenesis of keloids continues to be a subject of ongoing research. Current clinical efforts focus on optimizing therapeutic strategies based on existing evidence. In most cases, a multimodal treatment approach yields the best outcomes and contributes to the suppression of excessive proliferative growth.
Keypoints
-
Keloids need to be distinguished from hypertrophic scars.
-
Keloid pathophysiology is complex, multifactorial and still not completely understood.
-
No single treatment is universally efficient – a multimodal treatment approach is key.
-
Skin type, location and patient adherence significantly influence treatment success.
What are keloids?
Keloids are elevated, bulky scars or papules that can vary in color, ranging from erythematous to violaceous or brown pigmentation.1 In contrast to hypertrophic scars, keloids are clinically more severe, often causing increased pruritus and pain.1,2 While hypertrophic scars remain within the boundaries of original scar edges, keloids extend beyond (Fig. 1). Keloids are characterized by a random arrangement and disorganized septal structure of type I and III collagen fibers.1,2 They typically develop months to years after the initial injury or wound healing process, further distinguishing them from hypertrophic scars, which form within weeks.
Potential triggers include surgical incisions, burns, trauma wounds, piercings, insect bites, folliculitis, herpes zoster, vaccinations and acne. It has also been noted to occur following facial dermabrasion in patients undergoing isotretinoin therapy.1 Risk factors can include a family history of keloids, darker skin types (especially in African and Asian ethnic groups), pregnancy, puberty and skin injuries occurring over areas with bony prominences.1,4
Keloid pathophysiology
There are 4 primary phases of healing when skin is wounded: hemostasis, inflammation, proliferation and remodeling. Early in the healing process, inflammatory cells, fibroblasts and epithelial cells are recruited. A balance between collagen production, degradation and extracellular matrix (ECM) are crucial for proper scar formation.1
Imbalances can lead to excessive proliferation, which is theorized to be the cause of keloid development.1,2 This seems to be mediated by an overactivation of keloid fibroblasts due to an increased inflammatory environment, especially through dysregulated levels of three transforming growth factor-beta isoforms (TGF-β1, TGF-β2, TGF-β3).1 An overproduction of cytokines,3 along with other inflammatory proteins such as vascular-endothelial growth factor (VEGF) and platelet–derived growth factor (PDGF).2,4 is believed to contribute to the overproduction of collagen as well.2 Some investigators have reported the presence of mast cells and histamine in keloid tissue, which could explain the pruritus associated with it.4
In contrast to normal tissue, keloids have shown to be more metabolically active and to use more oxygen, which leads to a state of hypoxia in keloid fibroblasts.4 Recent studies suggest that keloid fibroblasts may differ from normal fibroblasts in actin filament stiffness and force generation, possibly driving their growth beyond the wound. They also seem to produce excess ECM on rigid substrates, partly explaining the higher risk of keloid formation in high-tension areas like chest and upper back.1
Other potential mechanisms that may contribute to keloid forming, including mutations in multiple loci across various chromosomes,1,4 microRNA-21 signaling pathways, histone modification, regulatory RNA alternations and DNA methylation, need to be further investigated.1
Treatment options for keloids
Silicone gel sheeting
Silicone gel sheeting (SGS) is believed to work through occlusion and hydration of the wound bed.2,4,8 Scar tissue tends to lose more water through the epidermis, which may indicate a weakened water barrier in the stratum corneum. The SGS helps retain moisture, preventing the stratum corneum from drying out, which in turn reduces the activation of fibroblasts and collagen production.2 For optimal efficacy, the sheets should be worn continuously for a minimum of 12 hours per day over several months following excision.4,5,8 The use of silicone preparations postoperatively for the prophylaxis of de novo keloid formation in predisposed individuals, as well as after surgical treatment of keloids, can be recommended.5
Pressure garment therapy
A correlation has been established between wound tension and the pathogenesis of keloid formation.6 Applying pressure and reducing wound tension have shown promising results in lowering recurrence rates especially after excision and combined with other treatment options, if patients adhere to the treatment plan of wearing it at least 12 hours a day for a minimum of six months.2,6 It leads to a reduction in capillary perfusion, accelerates collagen maturation, and thereby flattens the scar.5 It is particularly recommended for large scars, as well as after surgical procedures with known tendency to hypertrophic scars or keloids.5
Triamcinolone acetonide
Triamcinolone acetonide (TAC) is a intralesional corticosteroid injection and still serves as a first-line treatment when it comes to keloid scars.1,2 It reduces inflammation and fibroblast proliferation, but promotes vasoconstriction and collagen degradation.1,4,6 It can be used as a sole therapy option or in combination with cryotherapy, as well as after surgical intervention.5 Recurrence rates vary between 9–50%, observing best results in keloid volume reduction with 2-week treatment intervals, unlike usual four-to-six-week intervals.4,6,7,8 Most common side effects include skin atrophy, telangiectasia and hypopigmentation (Fig. 2).1,7
Fig. 2: Keloid scar showing hypopigmentation and teleangiectasia as common side effects after triamcinolone acetonide 10mg injection
Surgery
Although surgery is a popular option in keloid treatment, recurrence rates are high (45–100%) and adjuvant therapies are necessary to avoid these elevated risks.2,8 The main objective here is to minimize wound tension by carefully approximating the wound edges,2 handling the tissue gently and facilitating a new healing process that allows for a wide range of treatment options.2,4 Timely immobilization and pressure/compression can assist with tension relief. Conservative therapies can complement recurrence prevention. Lipotransfer and therapy using the mesenchymal stem cells in adipose tissue are still in the experimental stage and are being further researched.5
Cryotherapy
Traditional cryotherapy uses freezing temperature to cause irreversible cellular damage followed by a necrosis of keloid tissue.2,8 In one study it modified collagen synthesis and supported fibroblast differentiation.4,6 Two approaches can be distinguished: short cryosurgery, especially in combination with TAC to facilitate its injection, or intensive cryotherapy with complete freezing of the tissue. Spray and contact methods, as well as intralesional cryosurgery, can be performed.5 However, persistent hypopigmentation has been observed in patients with Fritzpatrick skin types IV to VI. Recurrence rates vary from 0–24%.1,2
Radiotherapy
Literature shows that radiotherapy is most effective after surgical excision. It seems to reduce fibroblast proliferation and collagen synthesis.7 Postoperative radiation after the excision of a keloid should ideally begin within seven hours. Two application types can be distinguished:
-
Percutaneous radiation therapy
-
HDR (high dose rate)/LDR (low dose rate) brachytherapy: A plastic mini catheter is positioned at the deepest base of the surgical scar not more than 1cm below the skin. After closing the scar with sutures, a compression bandage should be applied.
HDR brachytherapy shows the lowest recurrence rates (average 10,5%), followed by LDR brachytherapy (average 21,3%), and then percutaneous radiation therapy (average 22,2%).5 The most common side effect was alteration in skin pigmentation (Fig. 3, Fig. 4).1,7,8
Fig. 3–4: Recurrent keloid formation on the ear helix following piercing and two prior excisions (above) and same keloid at four weeks post-surgery with eight completed percutaneous radiation therapy sessions (below)
5-Fluorouracil
5-Fluorouracil (5-FU) is a classic chemotherapeutic agent that is sometimes used off-label to treat keloids.5,8 It disrupts DNA replication and cellular proliferation.2 It has been shown to reduce fibroblast growth and TGF-β-driven collagen production,2,8 which in turn may reduce keloid scar height.2 Like TAC, 5-FU is strictly injected intralesional into the scar tissue using a syringe.5 Better outcomes were observed when combined with corticosteroid treatment,6,8 particularly in minimizing side effects of TAC treatment.1,7 Recurrence rates for the combination therapy have varied in most studies between 0–47%.7 Common side effects of 5-FU include pain, burning, hyperpigmentation and ulceration.4,8
Bleomycin
Bleomycin is a cytotoxic agent that induces apoptosis and sclerosis.1,8 It has been shown to decrease collagen synthesis by fibroblasts.2 As an off-label treatment, Bleomycin is particularly used in some countries for patients with darker skin. Compared to 5-FU, Bleomycin is thought to have a lower risk of causing skin ulcerations in darker-skinned patients. Bleomycin is injected directly into the scar tissue.5 Degrees of recurrence vary strongly between 0–50%.1 Common side effects are hyperpigmentation and skin atrophy.1,2,8
Mitomycin C
Mitomycin C, another off-label treatment for keloids, is an antibiotic agent with anti-neoplastic and anti-proliferative characteristics, inhibiting the synthesis of DNA, RNA and protein and thus fibroblast proliferation.1,2,8 It can reduce keloid recurrence when used topically post excision.1,2 Recurrence rates vary between 0–33% and reported side effects were hypopigmentation and post treatment pain.2
Laser
Laser therapy uses controlled light energy, delivered at specific wavelengths and pulse durations to precisely target and break down selected tissue.4 In this section, we categorize lasers into ablative and non-ablative types. Ablative lasers work by removing the epidermal layer of the skin, whereas non-ablative lasers bypass the epidermis and target the dermis directly, aiming at the chromophore within the dermis.1
Ablative lasers
Ablative lasers include the carbon dioxide (CO2) laser, erbium-doped yttrium aluminium garnet (Er:YAG) laser, erbium-doped yttrium scandium gallium garnet (Er:YSGG) and thulium laser. While CO2 and Er:YAG lasers are commonly used for scar revision, evidence for their effectiveness on keloids is limited. They both target water in tissues to promote collagen remodeling. They can be used for superficial ablation or surgical excision of keloids. Multiple sessions have shown improvements in scar pliability, itching, pigmentation, redness and thickness.2,5 However, recurrence remains high after single treatments and without additional therapies. Especially carbon dioxide lasers have not shown high efficacy.4 Adjunctive treatments like steroids may improve outcomes.2 Guidelines suggest that for non-active keloids a treatment with an ablative laser in combination with TAC or laser-assisted drug delivery may be considered for the treatment of flat keloids.5 Common side effects for both, but especially for CO2 lasers, are de- and hyperpigmentation. Another technique uses radiofrequency-assisted fractional thermolysis prior to drug application. This allows the therapeutic agent to reach the full depth of the lesion.9 Studies show various outcomes in recurrence rates. Further studies are necessary to explore the effectiveness of laser-assisted drug delivery for keloid treatment (Fig. 5–8).2
Fig. 5–6: Spontaneous keloid formation on the sternum in a patient with prior history of acne (above). Same Patient after two sessions of fractional radiofrequency, each followed by intralesional injections of triamcinolone acetonide 10mg (below)
Fig. 7–8: Keloid formation in a patient with acne corporis six months after initiating isotretinoin therapy (above). Same patient after three sessions of fractional radiofrequency and simultaneous acoustic wave therapy (below)
Non-ablative lasers
Non-ablative lasers include the neodymium-doped yttrium aluminium garnet (Nd:YAG) laser, pulsed dye laser (PDL), potassium titanyl phosphate (KTP) laser and erbium glass laser (Er:Glass). The PDL operates at a wavelength of 585–595nm. It is designed to target the microvascular system by selectively damaging it, leading to localized hypoxia and reduced nutrient supply. Hemoglobin and oxyhemoglobin serve as the primary chromophores for this process. Several theories have been proposed to explain these effects, including the disruption of collagen disulfide bonds and elevated collagenase activity, though none have been definitively confirmed.2 Guidelines recommend its use primarily for erythema reduction in fresh, vascularized hypertrophic scars and keloids.5 Intense pulsed light (IPL) may serve as an alternative to PDL therapy for targeting vascular lesions. KPT lasers, with a similar wavelength of 532nm, also offer effective treatment. Both KTP and PDL target key chromophores such as oxyhemoglobin and melanin, which can increase the risk of dyspigmentation, especially in patients with darker skin tones.10
The Nd:YAG 1064nm laser damages deep dermal vessels with subsequent reduction in collagen production by fibroblasts5 and redness. It may be a suitable choice for individuals with darker skin tones (Fitzpatrick types IV to VI) and, through its deeper penetration, for erythema reduction in thicker keloids.1,5
Interferons
Interferons have immunoregulatory, antifibrotic and antiproliferative functions.2 The two treatment options, Interferon α-2b and Interferon γ, are observed at decreased concentrations in keloids.1 Both suppress collagen production and scar contraction. Although many studies suggest no higher efficacy in comparison to placebo, there is one larger study (n=124) showing a recurrence rate of 18,7% when injected after excision. Side effects are mostly flu-like symptoms.8 The treatment remains controversial.
Onion extract (Allium cepa)
In animal model scars, it improves dermal collagen organization, and its derivate (quercetin) has antiproliferative, antihistamine1 and collagen-suppressive8 effects. External application should generally be done several times a day, preferably with gentle massage of the scar tissue. The treatment usually lasts for several weeks to months.5 It could be a good adjuvant therapy to TAC and SGS.1
Botulinum toxin A
Botulinum toxin A is known for its relaxing effect on muscle tension and thereby wound tension. It reduces also fibroblast proliferation and alters collagen activity during scar formation. Its use in keloid treatment remains uncertain.1
Imiquimod
Imiquimod 5% cream is a topical immunomodulatory treatment.1 It induces pro-inflammatory agents, especially IFNα, TNFα, IL-1. IL-6, IL-8 and IL-12, as well as apoptotic genes in keloid fibroblasts. It decreases excessive collagen production with a post excision recurrence rate of 24,7%.1,4,8 Its efficacy remains in question. Side effects include skin erosion, pain and hyperpigmentation.4,8
Conclusion
The availability of numerous treatment options shows that a gold standard for keloid management has yet to be determined.
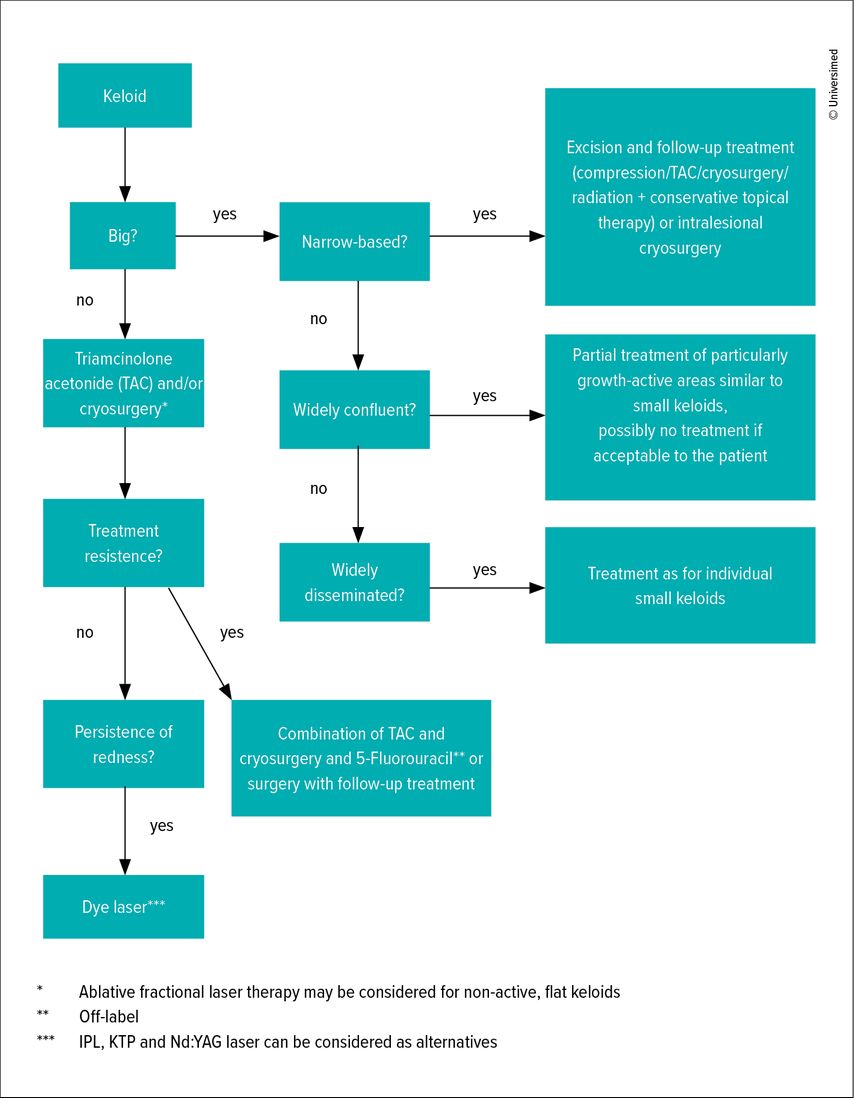
Therapy goals should be personalized and primarily focus on the patient’s concerns. Depending on the treatment option, a noticeable improvement – such as a volume reduction of 30–50%, a symptom reduction of >50%, and/or sufficient patient satisfaction – should be achieved after 3–6 treatments or after 3–6 months of therapy. If a satisfactory treatment outcome is not achieved within this time frame, it is recommended to adjust the treatment strategy, whether by combining methods, changing the approach, or increasing the dosage. None of the available methods for scar therapy can achieve scar reduction or improvement in all cases. Often, a combination of different treatment methods is required (Fig. 9).5
Due to the lack of a universally accepted gold standard, our clinic follows a personalized approach to keloid management. For patients with extensive or multiple keloids, we generally try different treatment options on selected lesions, preferably using vascular laser therapy and fractional radiofrequency. In cases of active and pruritic keloids, we additionally administer TAC injections at intervals of every three to four weeks to help manage inflammation and symptoms. Among these, both our medical team and patients have consistently observed the most noticeable improvements following fractional radiofrequency treatment, often after just a single session. Despite these clinical observations, the current scientific literature on fractional radiofrequency for keloid treatment remains limited and further research is necessary to substantiate its long-term efficacy.
Literatur:
1 Ekstein SF et al.: Keloids: a review of therapeutic management. Int J Dermatol 2021; 60(6): 661-71 2 Betarbet U, Blalock TW: Keloids: a review of etiology, prevention, and treatment. J Clin Aesthet Dermatol 2020; 13(2): 33-43 3 McGinty S, Siddiqui WJ: Keloid. Treasure Island (FL/USA): StatPearls Publishing, 2023 4 Chike-Obi CJ et al.: Keloids: pathogenesis, clinical features, and management. Semin Plast Surg 2009; 23(3): 178-84 5 Nast A et al.: S2k-Leitlinie Therapie pathologischer Narben (hypertrophe Narben und Keloide) – Update 2020. J Dtsch Dermatol Ges 2021; 19(2): 312-27 6 Walsh LA et al.: Keloid treatments: an evidence-based systematic review of recent advances. Syst Rev 2023; 12(1): 42 7 Thornton NJ et al.: Keloid Scars: An updated review of combination therapies. Cureus 2021; 13(1): e12999 8 Kim SW: Management of keloid scars: noninvasive and invasive treatments. Arch Plast Surg 2021; 48(2): 149-57 9 Choudhary R et al.: Radiofrequency-assisted fractional thermolysis for drug delivery in keloids. Indian J Dermatol Venereol Leprol 2024; 90(6): 842-3 10 Bronte J et al.: A comprehensive review of non-surgical treatments for hypertrophic and keloid scars in skin of color. Clin Cosmet Investig Dermatol 2024; 17: 1459-69
Das könnte Sie auch interessieren:
Kombinationstherapie mit plättchenreichem Plasma und Hyaluronsäure
Hochwertiges autologes plättchenreiches Plasma (PRP) verfügt von Natur aus über einen komplex zusammengesetzten Cocktail aus zahlreichen bioaktiven Substanzen. Gegenüber dem Vollblut ...
Chronische Wunde – Alltag im Ausnahmezustand?
Chronische Wunden sind nicht nur ein medizinisches, sondern auch ein „alltägliches“ Problem. Sie durchbrechen Routinen, verändern das Selbstbild und verlangen von den Betroffenen eine ...
Die menschliche Haut in der modernen Kunst
Dr. Ralph Ubl, Professor für neuere Kunstgeschichte an der Universität Basel, stellte sich der schwierigen Herausforderung, einem Raum voller erwartungsvoller Dermatologen das Organ Haut ...