Dermatopathology: what’s new?
Bericht:
Dr. med. Lydia Unger-Hunt
Vielen Dank für Ihr Interesse!
Einige Inhalte sind aufgrund rechtlicher Bestimmungen nur für registrierte Nutzer bzw. medizinisches Fachpersonal zugänglich.
Sie sind bereits registriert?
Loggen Sie sich mit Ihrem Universimed-Benutzerkonto ein:
Sie sind noch nicht registriert?
Registrieren Sie sich jetzt kostenlos auf universimed.com und erhalten Sie Zugang zu allen Artikeln, bewerten Sie Inhalte und speichern Sie interessante Beiträge in Ihrem persönlichen Bereich
zum späteren Lesen. Ihre Registrierung ist für alle Unversimed-Portale gültig. (inkl. allgemeineplus.at & med-Diplom.at)
Current insights include the fact that PRAME («preferentially expressed antigen in melanoma») is unfortunately not a perfect marker, but still very useful in borderline lesions; the warning that certain breast cancer types may mimic a melanoma in situ; and a helpful immunostain called NUT to differentiate between cutaneous cancers.
We can’t talk about updates in dermatopathology without talking about PRAME – it is an absolute hot topic”, states dermatopathologist Jerad M. Gardner, MD, head of the Department of Soft Tissue Pathology at Geisinger Medical Center in Danville, Pennsylvania.
PRAME: no magic bullet
First up, this preferentially expressed antigen in melanoma is – unfortunately – not a perfect magic bullet for deciding if a lesion is a melanoma or not. However, evidence shows that most melanomas (but not all) have diffuse PRAME expression, meaning that 75% of the lesion of melanocytes are positive. Subtypes, such as the superficial spreading melanoma, are 92.5% positive, acral melanoma are 89.3–94.4% positive. According to literature, there are two exceptions to this rule. Firstly, the subtype of spindle cell melanoma is only positive in 56% of cases, but Gardner “almost never” uses PRAME in these cases anyway, as spindle cell melanoma are “so ugly microscopically as to be obviously malignant”; all that is required here is melanocyte-proof with MART 1 or SOX10- markers.
The other exception is desmoplastic melanoma, which is sometimes lumped together with spindle cell melanoma. However, these two are very different: They look different, stain differently and show different clinical behavior, explains the expert: “Spindle cell melanoma act similarly to most other melanomas, while desmoplastic melanoma have a lower risk of metastasis on a depth-by-depth basis.” If PRAME is negative, it does not exclude desmoplastic melanoma, hence it should not be used as stand-alone diagnostic marker.
In Spitzoid melanocytic lesions and cases of intermediate histology, PRAME is more variable, with a good specificity of 93.5–100%, but a sensitivity of between 67–91.7%. “It is well known that PRAME can be positive in Spitzoid lesions with Spitz-type molecular abnormalities and in melanocytomas – it is not necessarily indicative of malignancy in that context.” In these cases, PRAME should be used “very cautiously” and NGS (“next-generation sequencing”) molecular testing can be helpful, especially for atypical Spitzoid lesions.
Avoid PRAME in obvious cases
There are also instances where PRAME should be avoided like the proverbial plague, and that is when a lesion is either obviously malignant or obviously benign. Why? “Because some obvious malignant melanomas are PRAME-negative, and some obvious benign nevi are PRAME-positive – and then what happens? You send it to an expert, order extra stains – basically stain yourself into a hole. I’m guilty of that myself, but as a hint: Don’t do it. You might get an answer you do not want to hear.”
Another thing worth remembering is that PRAME is not a pure melanoma marker, but can stain a variety of other neoplasms. “Just because a tumor is PRAME-positive that doesn’t automatically imply the diagnosis of a melanoma.” It could also be a poorly differentiated carcinoma, an angiosarcoma or a rhabdomyosarcoma; malignant peripheral nerve sheath tumors (MPNST) in turn are also often positive, but “despite popular belief they almost never occur in the skin. They are – with extremely rare exceptions – usually deep cell tissue tumors”, says Gardner.
So when should you use PRAME? “I use PRAME on borderline lesions, where I’m not completely sure if it is benign or malignant. As mentioned, it is not a perfect 100% marker, just an extra tool in the toolkit.” PRAME is also useful for melanoma in situ arising in nevus vs invasive nevoid melanoma to help decide if the dermal component is melanoma and to measure Breslow thickness. But in general, diagnostics should always factor in the context of clinical characteristics, pathology and the immunostaining in one big picture as well, “and make sure it makes sense”. And this is also the reason why Gardner thinks that artificial intelligence – whilst being very helpful in this field – will not completely replace his particular job in the near future. (“And if it does, we will have much bigger problems, such as the ones showcased in ‘The Matrix’ or in ‘Terminator’ – problems when you have to worry about society, rather than wondering how to keep your job.”)
For those interested in a deep dive, Gardner recommends a recently published review of PRAME and a paper on undifferentiated and dedifferentiated melanomas.1,2 The latter study showed strong and diffuse nuclear PRAME staining for both primary and metastatic dedifferentiated and undifferentiated melanomas, as well as in all conventional melanoma precursors (except for desmoplastic melanoma); by contrast, PRAME staining in atypical fibroxanthoma and pleomorphic dermal sarcoma was patchy and weak.2 These data emphasize the diagnostic utility of PRAME staining as a first screening tool in the detection and workup of dedifferentiated and undifferentiated melanomas, indicating PRAME as “helpful supporting feature in that rare but very challenging diagnostic scenario”, comments the expert.
Breast carcinoma mimicking melanoma
The next topic is SOX10 (Sry-related HMg-Box gene 10), a key nuclear transcription factor in the differentiation of neural crest progenitor cells to melanocytes, and a sensitive and specific marker of malignant melanoma of multiple histologic types. However, breast carcinomas are also often SOX10-positive – “something that I only learned a few years ago, which is shocking”, admits Gardner. Breast pathologists often use SOX10 in the setting of poorly differentiated spindle cells or metaplastic breast carcinomas, because they tend to begin to lose their keratin expression, but will usually be positive for SOX10. This is very important for dermatopathologists to know, “because we are so used to thinking of the equation of ‘SOX10 plus malignant = melanoma’”. And in 99% of the time, this equation would be correct, but it is vital to remember the 1% exception, especially as the corresponding therapies are “really quite different”. A recently published “unique” case report of a triple-negative breast carcinoma (TNBC) metastatic to the skin exhibited histopathologic characteristics similar to melanoma, including positivity for SOX10 and PRAME – a “diagnostic pitfall”, as Gardner calls it.
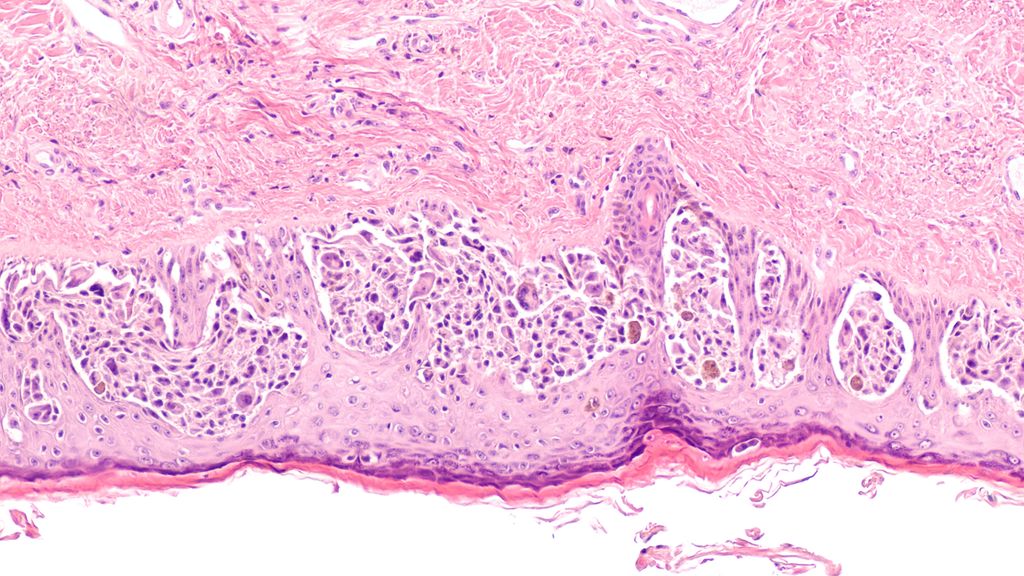
SOX-10 may often be positive in breast carcinoma, but surely “breast carcinoma does not look like melanoma on H&E, right?” Well, no – but some breast carcinomas can mimic melanoma. An overview:
-
Paget disease of the nipple + SOX-10-positive = melanoma in situ mimic
-
Basal-like breast carcinoma triple negative + SOX-10-positive = melanoma in situ mimic
-
Metaplastic (spindle cell/sarcomatoid) breast carcinoma (in skin or distant metastasis) + SOX-10-positive = spindle cell melanoma mimic. To complicate diagnostics even further, metaplastic/spindle cell breast carcinoma is also triple negative for ER/PR/Her2.
This knowledge is, again, of huge importance, due to the “very, very different” systemic therapies for breast cancer and melanoma.
SOX11 and NUT stains
SOX11 on the other hand can be used as a marker for the distinction between Merkel cell carcinoma (MCC) and pulmonary small cell carcinoma (PSmCC), as another paper showed.4 The differentiation between these two tumors is challenging even with immunohistochemistry such as TTF1, as they can occasionally lack classic immunophenotypes, write the authors. In their study, SOX11 expression was present in all MCCs, but much less commonly in PSmCCs (25%); as an added bonus, SOX11 expression was more likely than CK20 expression to be strong or diffuse in sentinel lymph node (SLN) metastases of MCC. According to the authors, this indicates that SOX11 is superior to CK20 for detecting tumor deposits in SLNs in MCC.
Last but not least, the topic is NUT carcinomas: NUT1 (“nuclear protein in testis”) is a gene, and an immunostain called NUT is positive in a rare type of internal carcinoma known as NUT midline carcinoma, “a very aggressive tumor with a very poor outcome”. As it turns out, some cutaneous tumors – both benign and malignant – also express NUT, but lack the aggressive behavior. This was first observed in poroid neoplasms, a subset of which have NUTM1 gene fusions, usually with YAK1 as the partner gene. A study on NUT immunohistochemical expression encompassing 835 cases of various cutaneous epidermal or adnexal epithelial neoplasms showed that NUT expression was specific to eccrine poromas and porocarcinoma, with 32% of cases showing NUT expression.5 All other cutaneous tumors tested lacked NUT expression, including Bowen disease or squamous cell carcinoma. “This observation is helpful”, as these tumors – poroid carcinoma, Bowen’s disease, squamous cell carcinoma – “can often look quite similar”.
In any case, it is “really amazing that genetics and molecular open up so many doors and answer questions, but also ask so many new questions”, concludes Gardner. In practice however, “I just know enough to recognize what tests to order. And when it gets really complicated – I just ask my molecular colleagues to help me out”.
Melanoma and PRAME pitfalls
Some obvious malignant melanomas are PRAME-negative.
Some obvious benign nevi are PRAME-positive.
In obvious cases: Don’t do PRAME!
Some other tumors may stain with PRAME (MPNST, rhabdomyosarcoma, breast carcinoma).
Cave melanoma mimics: Paget disease of nipple, triple-negative or metaplastic breast carcinoma in skin or positive for distant metastasis + SOX-10.
Source:
„Whatʼs new? Updates in Dermapathology“, Jerard M. Gardener, MD, SGDV-Jahrenskongress 2024, 20. September 2024, Basel
Literature:
1 Bourgeau M, Gardner JM: Immunohistochemistry update in dermatopathology and bone and soft tissue pathology. Arch Path Lab Med 2024; 148(3): 284-91 2 Hornick JL et al.: PRAME expression is a useful tool in the diagnosis of primary and metastatic dedifferentiated and undifferentiated melanoma. Am J Surg Pathol 2023; 47(12): 1390-7 3 Fliorent R et al.: Metastatic triple-negative breast carcinoma mimicking melanoma: A potential diagnostic pitfall. J Cutan Pathol 2024; 51(9): 654-7 4 Cho WC et al.: SOX11 is an effective discriminatory marker, when used in conjunction with CK20 and TTF1, for merkel cell carcinoma: comparative analysis of SOX11, CK20, PAX5, and TTF1 expression in merkel cell carcinoma and pulmonary small cell carcinoma. Arch Pathol Lab Med 2023; 147(7): 758-66 5 Macagno N et al.: NUT is a specific immunohistochemical marker for the diagnosis of YAP1-NUTM1-rearranged cutaneous poroid neoplasms. Am J Surg Pathol 2021; 45(9): 1221-7
Das könnte Sie auch interessieren:
Mikrotoning – sanfte Behandlung mit Effekt?
Erweiterte Kapillargefässe sind ein weitverbreitetes und kosmetisch störendes Phänomen. Manchmal sind sie schon mit blossem Auge sichtbar oder erweitern sich anfallsartig, wodurch eine ...
«Wir reden in der Medizin zu wenig über Sex»
Wer im Kontext von Haut und Sexualität primär an sexuell übertragbare Infektionen (STI) denkt, könnte überrascht werden. Denn das Thema Sexualität ist gesundheitlich aus ganz ...
Die menschliche Haut in der modernen Kunst
Dr. Ralph Ubl, Professor für neuere Kunstgeschichte an der Universität Basel, stellte sich der schwierigen Herausforderung, einem Raum voller erwartungsvoller Dermatologen das Organ Haut ...


